New research enables first successful treatment of pediatric high-risk refractory neuroblastoma with PARP inhibition
Scientists and clinicians at St. Jude Children’s Research Hospital identified the genetic vulnerability BARD1 in a patient with pediatric neuroblastoma, successfully treating the disease with targeted therapy.
St. Jude Children’s Research Hospital scientists report the first successful treatment of a pediatric patient with high-risk refractory neuroblastoma using a targeted therapy guided by clinical genomics. Poly (ADP-ribose) polymerase (PARP) inhibition successfully exploited an identified genetic vulnerability in the patient’s cancer. The vulnerability was a mutation in the BARD1 gene, causing a defect in a DNA damage repair pathway. PARP inhibition, in combination with chemotherapeutics, exploited the cancer’s DNA damage repair defect, eventually leading to the malignancy’s destruction. The report was published today in The New England Journal of Medicine.
“At the time the patient came to St. Jude, multiple therapies had failed them,” said co-corresponding author Sara Federico, MD, St. Jude Department of Oncology, Division of Solid Tumor director. “Once we identified their specific BARD1 mutation, we were able to give them targeted therapy and eradicate their cancer. We were thrilled to see a dramatic clinical response. The patient has been off therapy for more than two years now. This treatment regimen may be successfully used for other patients with BARD1 mutations in the future.”
Refractory neuroblastoma, which resists frontline conventional treatment, is a high-risk disease with a poor prognosis. The St. Jude team used germline DNA and RNA sequencing to look for new vulnerabilities in the patient’s cancer that could be targeted therapeutically. Analyzing the data led to identifying BARD1 as driver mutation in this patient’s cancer.
“Understanding the genetic basis of an individual cancer, in this patient the complete loss of BARD1 in the tumor, led to the impressive clinical outcomes observed after PARP inhibition,” said co-corresponding author Jinghui Zhang, PhD, Endowed Chair of Bioinformatics, St. Jude Department of Computational Biology. “This case report demonstrates the potential impact of multi-omics analysis of RNA and DNA in the clinical setting. Such computational analysis is critical to assess target vulnerability and pediatric patient eligibility for precision treatments such as PARP inhibition.”
Treatment history and molecular features of a high-risk neuroblastoma patientwith sustained response to PARP inhibitor (talazoparib)
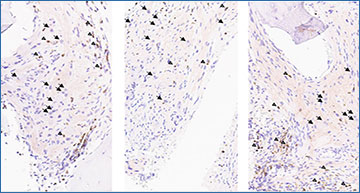
a) Patient’s (patient ID SJNBL031647) bone marrow response over time in months, depicted by bone marrow biopsy histology (top row) and response per Revised INRC Criteria (middle rows), in correlation with treatments received over time (bottom rows), demonstrated by colored horizontal bars. b) Allele-specific expression of BARD1 in tumor RNA-seq of the index patient (SJNBL031647). c) BARD1 protein expression in index patient’s tumor cells at months 0, 2 and 4. d) Synthetic lethality (SL) score was estimated by a pediatric cancer-based gene network model for PARP1 and PARP2 inhibition.
After uncovering BARD1’s involvement, the oncologists adapted treatment to PARP inhibitor talazoparib in combination with irinotecan. Talazoparib is already Food and Drug Administration approved for use in different indications adults. The pediatric patient has been off therapy for over two and a half years with no detectable disease, making this the first report of a neuroblastoma patient with a BARD1 mutation successfully treated with PARP inhibition. This provides rationale for future treatments to target vulnerabilities in DNA damage response genes in solid tumors.
Source – St. Jude Children’s Research Hospital
