Northwestern Medicine investigators have discovered that uterine serous carcinoma tumors in Black patients express more aggressive and immunosuppressive features than tumors in white patients, according to a recent study published in the Proceedings of the National Academy of Sciences.
The findings may inform new targeted therapeutic strategies to improve disparities in patient outcomes, according to Julie Kim, PhD, the Susy Y. Hung Research Professor of Obstetrics and Gynecology in the Division of Reproductive Science in Medicine, and senior author of the study.
“Our environment, our behaviors, societal stressors, they all impact us psychologically as well as physically. If the environmental insults are chronic, or if they’re too much to bear, it can have an impact on health,” Kim said. “We are seeing differences in these tumors in terms of the genes that they express, in terms of the immune system and the immune response.”
Uterine serous carcinoma (USC) is a rare and aggressive type of endometrial cancer, comprising up to 10 percent of all primary endometrial cancer cases, according to the Foundation for Women’s Cancer. The five-year survival rate for patients with advanced cancer is around 30 percent.
The cancer also disproportionately affects Black women, with previous research having shown differences in cancer driver mutations in tumors from Black patients compared to white patients.
“There is indeed a racial disparity in endometrial cancer, in that Black women with this cancer suffer from higher mortality rates,” Kim said.
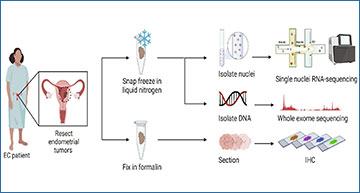
In the current study, the scientists aimed to better understand the molecular and genomic differences in USC tumors between Black patients and white patients by performing single-nuclei RNA sequencing of USC tumor samples from four white patients and nine Black patients.
“These tumors are very rare, and so it’s difficult to get samples. We had to rely on tumor banks that have been established to obtain these samples,” Kim said.
From these samples, the investigators discovered that tumors from Black patients demonstrated increased expression of genes associated with tumor aggressiveness – notably PAX8, which is commonly upregulated in other endometrial cancers and in ovarian cancer – compared to white patients.
Patients with tumors with increased PAX8 expression also had worse overall survival compared to patients with low PAX8 expression, according to the authors.
Furthermore, they discovered that PAX8 directly influences the activity of macrophages – specialized white blood cells that kill cancer cells and stimulate other immune cells – within the USC tumor microenvironment to suppress anti-tumor immune responses, and that this was more prevalent in tumors from Black patients.
“This is the first time PAX8 has been investigated for its involvement with immune signaling. Hopefully, this work can contribute to our understanding of endometrial cancer and improve survival for these patients,” said Grace Foley, a student in the Driskill Graduate Program in Life Sciences (DGP) and lead author of the study.
The findings underscore the clinical relevance of PAX8 upregulation in USC, especially in Black patients, which may serve as a potential therapeutic target, according to Kim.
The next steps for the research, according to Kim, include duplicating their findings in a larger patient cohort and identifying current drugs that may help tumors with increased PAX8 expression better respond to the immune system.
“It’ll be important to test what we found in a larger cohort to make sure that this is indeed something that is fundamentally different between Black and white women,” Kim said. “We want to gather more data so that we can be confident in potentially testing compounds in preclinical studies before going towards clinical trials.”
Source – Northwestern Medicine
